A recombinant SARS-CoV-2 vaccine
NANBIOSIS Protein Production Platform (PPP) Unit 1 (of CIBER-BBN and Autonomous University of Barcelona) is involved in a micro-patronage project for the development of a vaccine for COVID 19.
NANBIOSIS Unit 1 is directly involved in the initial part of the Virus Like Particles and Proteins expression and purification project of SARS-COV-2
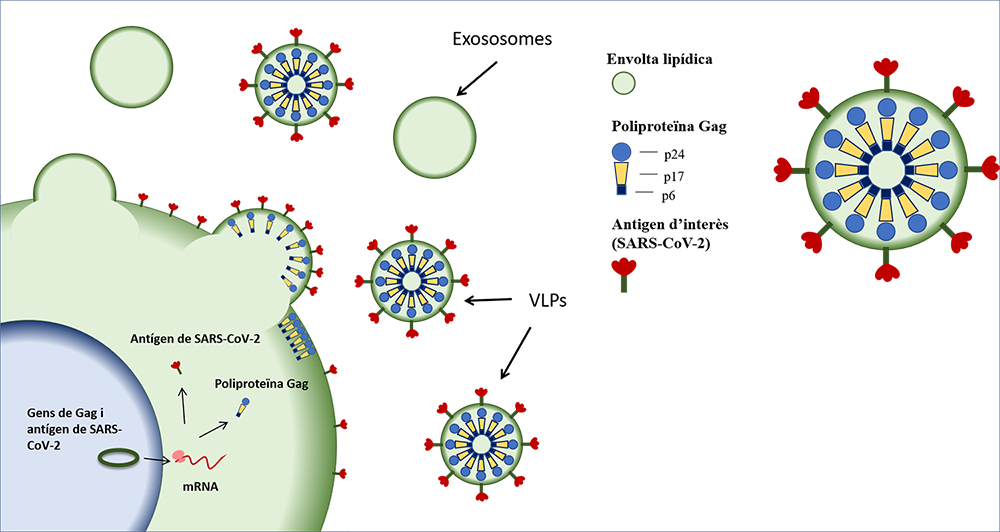
Most vaccines used today are based on either attenuated forms of the original pathogen, or are inactivated vaccines, in which the pathogen has undergone physical or chemical treatments to eliminate its infectivity. The project proposes to use a new vaccine strategy based on recombinant proteins in imitation of viruses (virus-like particles or VLPs). The same strategy with which, for example, papillomavirus and hepatitis B virus vaccines have been created.
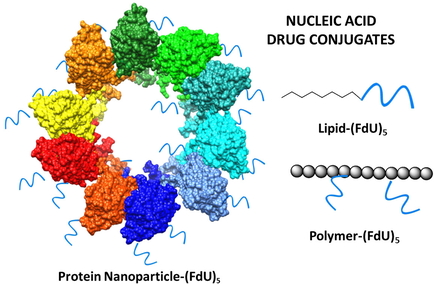
VLPs contain recombinant structural proteins, obtained by the introduction and expression of a gene in cultured cells, that form nanostructures similar to viral particles but do not contain their genetic information and, therefore, are not infectious. These particles are capable of arousing a strong immune response as they form a three-dimensional structure where the virus epitopes are exposed, but they are very safe.
VACCINE PROTOTYPE:
Design
First, we will design the genes that encode the structural proteins of the virus. At this point, the different sequences of the virus genome deposited in public databases must be analyzed and compared in detail. In this way, we can select the most representative sequence. On the other hand, we will carry out some control tests to detect the different fragments of the proteins where the response of the immune system is concentrated, the so-called antigens.
These studies will be carried out using bioinformatics tools by the Computational Biology Group of dr. Xavier Daura from the UAB Institute of Biotechnology and Biomedicine (IBB).
Production and purification
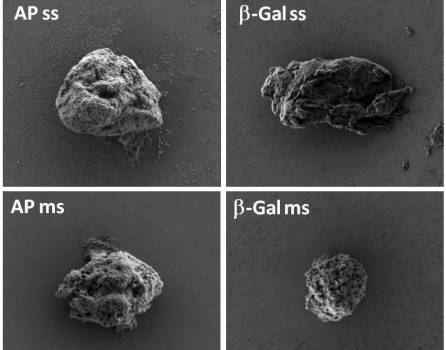
To carry out these productions, we need to use cultured cell lines in which we introduce the genes that encode the virus’s proteins and establish optimal obtaining conditions, without the need to use highly biological containment laboratories. Once produced, we will carry out a purification process and they can be validated.
This block will be carried out in parallel by the research group led by Dr. Francesc Godia from the Department of Chemical, Biological and Environmental Engineering, and Dr. Neus Ferrer from the Department of Genetics and Microbiology and member of the Nanobiotechnology Group led by Dr Antoni Villaverde, attached to the IBB and the CIBER-BBN. In addition, we will have the help of UAB research-scientific-technical services, such as the Microscopy Service (SM), and the Proteomics and Structural Biology Service (sePBioEs) and a unique scientific-technical infrastructure called NANBIOSIS.
Validation with patient serum and cell models
Once the proteins are purified, it is necessary to validate the vaccine formulations with patient serum. In other words, it must be demonstrated that the patient sera of the COVID-19 are linked to the vaccine proposals developed. This task will be coordinated by dr. Eduard José Cunilleras from the UAB Department of Animal Medicine and Surgery in collaboration with doctors from the Parc Taulí, Germans Trias, Vall d’Hebron and Santa Creu i Sant Pau hospitals, and the help of the scientific-technical service to support the research of the Crop, Antibody and Cytometry Service (SCAC) of the UAB.
TESTS ON ANIMALS
Any product to be administered to humans must first go through a preclinical phase in animal models. All trials, when they reach this stage, must be approved by the Ethics Committee on Animal and Human Experimentation. The safety and efficacy of the vaccine are tested in these models.
During vaccination trials we will monitor the weight of the animals and their general condition. The presence of antibodies in the blood of vaccinated animals will be evaluated in cell cultures. The serum of the vaccinated animals will be incubated with the SAR-CoV-2 and we will proceed to the infection of cell cultures. If the antibodies are capable of reducing the infectivity of the virus, then we will move on to the final part of this stage, which will consist of infecting the vaccinated animals with the virus to see if they are protected from infection. A group of unvaccinated animals will also be infected and we will compare the results with another group of unvaccinated and uninfected animals. The vaccine should give similar results to the last group of animals.
Further information about the project and FAQs about donations: https://micromecenatge.uab.cat/vacunacoronavirus